Вирус Эбола (Filoviridae: Ebolavirus: Zaire ebolavirus): фатальные адаптационные мутации
- Авторы: Должикова И.В.1, Щербинин Д.Н.1, Логунов Д.Ю.1, Гинцбург А.Л.1
-
Учреждения:
- ФГБУ Национальный исследовательский центр эпидемиологии и микробиологии имени почётного академика Н.Ф. Гамалеи Минздрава России
- Выпуск: Том 66, № 1 (2021)
- Страницы: 7-16
- Раздел: ОБЗОРЫ
- URL: https://journal-vniispk.ru/0507-4088/article/view/118145
- DOI: https://doi.org/10.36233/0507-4088-23
- ID: 118145
Цитировать
Аннотация
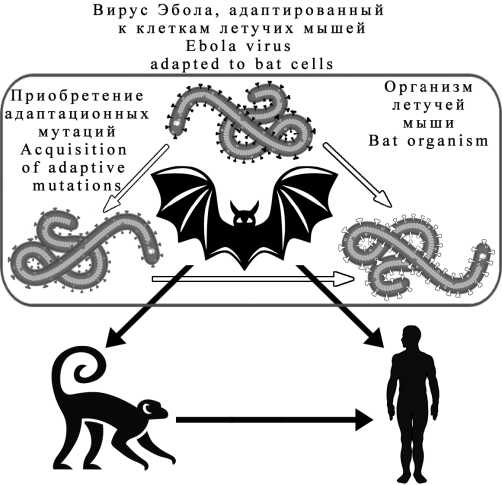
Болезнь, вызванная вирусом Эбола (БВВЭ) (прежнее название - геморрагическая лихорадка Эбола), - одно из самых опасных инфекционных заболеваний, поражающих человека и приматов. С момента идентификации первой вспышки в 1976 г. в мире зарегистрировано более 25 аналогичных эпизодов, самый крупный из которых в 2014-2016 гг. перерос в эпидемию и унёс жизни свыше 11 тыс. человек. В настоящее время одновременно в восточной и западной частях Демократической Республики Конго (ДРК) протекают 2 независимые вспышки БВВЭ. Считается, что естественным резервуаром её возбудителей являются летучие мыши (Microchiroptera), однако инфекционный агент из них до сих пор не выделен. Известно, что большинство вирусов животных не способно реплицироваться в человеческом организме. Для того чтобы произошло заражение человека, необходимо наличие адаптационных мутаций (АМ). В данном обзоре на основании результатов ряда исследований сформулирована гипотеза о том, что формирование мутационных изменений подобного рода происходит непосредственно в популяциях людей и приматов, приводя в дальнейшем к развитию вспышек БВВЭ.
Ключевые слова
Полный текст
Открыть статью на сайте журналаОб авторах
И. В. Должикова
ФГБУ Национальный исследовательский центр эпидемиологии и микробиологии имени почётного академика Н.Ф. Гамалеи Минздрава России
Автор, ответственный за переписку.
Email: dolzhikova@gamaleya.org
ORCID iD: 0000-0003-2548-6142
Должикова Инна Вадимовна - кандидат биологических наук, заведующая лабораторией Государственной коллекции вирусовю
123098, Москва
РоссияД. Н. Щербинин
ФГБУ Национальный исследовательский центр эпидемиологии и микробиологии имени почётного академика Н.Ф. Гамалеи Минздрава России
Email: dim284@inbox.ru
ORCID iD: 0000-0002-8518-1669
Щербинин Дмитрий Николаевич - кандидат биологических наук, научный сотрудник лаборатории молекулярной биотехнологии.
123098, Москва
РоссияД. Ю. Логунов
ФГБУ Национальный исследовательский центр эпидемиологии и микробиологии имени почётного академика Н.Ф. Гамалеи Минздрава России
Email: ldenisy@yahoo.com
ORCID iD: 0000-0003-4035-6581
Логунов Денис Юрьевич - член-корреспондент РАН, заместитель директора.
123098, Москва
РоссияА. Л. Гинцбург
ФГБУ Национальный исследовательский центр эпидемиологии и микробиологии имени почётного академика Н.Ф. Гамалеи Минздрава России
Email: gintsburg@gamaleya.org
ORCID iD: 0000-0003-1769-5059
Гинцбург Александр Леонидович - доктор биологических наук, академик РАН, директор.
123098, Москва РоссияСписок литературы
- Sanchez A., Geisbert T.W., Feldmann H. Filoviridae: Marburg and Ebola viruses. In: Knipe D.M., Howley P.M., eds. Fields Virology. Philadelphia: Lippincott Williams & Wilkins; 2006: 1409-48.
- Taylor D.J., Leach R.W., Bruenn J. Filoviruses are ancient and integrated into mammalian genomes. BMC Evol. Biol. 2010; 10: 193. https://doi.org/10.1186/1471-2148-10-193.
- Geisbert T.W. Marburg and Ebola hemorrhagic fever (Filoviruses). In: Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Philadelphia: Elsevier; 2015: 1995-9.
- International Committee on Taxonomy of Viruses. Available at: https://talk.ictvonline.org/taxonomy/p/taxonomy-history?taxnode_id=201901569 (accessed January 14, 2021).
- Bharat T.A., Noda T., Riches J.D., Kraehling V, Kolesnikova L., Becker S., et al. Structural dissection of Ebola virus and its assembly determinants using cryo-electron tomography. Proc. Natl. Acad. Sci. USA. 2012; 109(11): 4275-80. https://doi.org/10.1073/pnas.1120453109.
- Ascenzi P., Bocedi A., Heptonstall J., Capobianchi M.R., Di Caro A., Mastrangelo E., et al. Ebolavirus and Marburgvirus: insight the Filoviridae family. Mol. Aspects Med. 2008; 29(3): 151-85. https://doi.org/10.1016/j.mam.2007.09.005.
- Gutsche I., Desfosses A., Effantin G., Ling W.L., Haupt M., Ruigrok R.W., et al. Structural virology. Near-atomic cryo-EM structure of the helical measles virus nucleocapsid. Science. 2015; 348(6235): 704-7. https://doi.org/10.1126/science.aaa5137.
- Beniac D.R., Booth T.F. Structure of the Ebola virus glycoprotein spike within the virion envelope at 11 A resolution. Sci. Rep. 2017; 7: 46374. https://doi.org/10.1038/srep46374.
- Wong G., He S., Leung A., Cao W., Bi Y, Zhang Z., et al. Naturally occurring single mutations in Ebola virus observably impact infectivity. J. Virol. 2018; 93(1): e01098-18. https://doi.org/10.1128/JVI.01098-18.
- Ruedas J.B., Arnold C.E., Palacios G., Connor J.H. Growth-adaptive mutations in the Ebola virus Makona glycoprotein alter different steps in the virus entry pathway. J. Virol. 2018; 92(19): e00820-18. https://doi.org/10.1128/JVI.00820-18.
- Ruedas J.B., Ladner J.T., Ettinger C.R., Gummuluru S., Palacios G., Connor J.H. Spontaneous mutation at amino acid 544 of the Ebola virus glycoprotein potentiates virus entry and selection in tissue culture. J. Virol. 2017; 91(15): e00392-17. https://doi.org/10.1128/JVI.00392-17.
- Kurosaki Y., Ueda M.T., Nakano Y., Yasuda J., Koyanagi Y., Sato K., et al. Different effects of two mutations on the infectivity of Ebola virus glycoprotein in nine mammalian species. J. Gen. Virol. 2018; 99(2): 181-6. https://doi.org/10.1099/jgv.0.000999.
- Diehl W.E., Lin A.E., Grubaugh N.D., Carvalho L.M., Kim K., Kyawe P.P., et al. Ebola virus glycoprotein with increased infectivity dominated the 2013-2016 epidemic. Cell. 2016; 167(4): 1088-98. e6. https://doi.org/10.1016/j.cell.2016.10.014.
- Ueda M.T., Kurosaki Y., Izumi T., Nakano Y., Oloniniyi O.K., Yasuda J., et al. Functional mutations in spike glycoprotein of Zaire ebolavirus associated with an increase in infection efficiency. Genes Cells. 2017; 22(2): 148-59. https://doi.org/10.1111/gtc.12463.
- Wang M.K., Lim S.Y., Lee S.M., Cunningham J.M. Biochemical basis for increased activity of Ebola glycoprotein in the 2013-16 epidemic. Cell Host Microbe. 2017; 21(3): 367-75. https://doi.org/10.1016/j.chom.2017.02.002.
- Dietzel E., Schudt G., Krahling V, Matrosovich M., Becker S. Functional characterization of adaptive mutations during the West African Ebola virus outbreak. J. Virol. 2017; 91(2): e01913-16. https://doi.org/10.1128/JVI.01913-16.
- Urbanowicz R.A., McClure C.P., Sakuntabhai A., Sall A.A., Kobinger G., Muller M.A., et al. Human adaptation of Ebola virus during the West African outbreak. Cell. 2016; 167(4): 1079-87.e5. https://doi.org/10.1016/j.cell.2016.10.013.
- wHo. Ebola Situation Report-21; 2015. Available at: https:// apps.who.int/ebola/current-situation/ebola-situation-report-21-october-2015 (accessed January 14, 2021).
- CDC. Ebola virus disease distribution map: Cases of Ebola virus disease in Africa since 1976. Available at: https://www.cdc.gov/vhf/ebola/history/distribution-map.html (accessed January 14, 2021).
- Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/ International Study Team. Bull. World Health Organ. 1978; 56(2): 247-70.
- Report of an International Commission. Ebola haemorrhagic fever in Zaire, 1976. Bull. WorldHealth Organ. 1978; 56(2): 271-93.
- Baize S., Pannetier D., Oestereich L., Rieger T., Koivogui L., Magassouba N., et al. Emergence of Zaire Ebola virus disease in Guinea. N. Engl. J. Med 2014; 371(15): 1418-25. https://doi.org/10.1056/NEJMoa1404505.
- CDC. 2014-2016 Ebola Outbreak in West Africa. Available at: https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html (accessed January 14, 2021).
- Mari Saez A., Weiss S., Nowak K., Lapeyre V, Zimmermann F., Dux A., et al. Investigating the zoonotic origin of the West African Ebola epidemic. EMBO Mol. Med. 2015; 7(1): 17-23. https://doi.org/10.15252/emmm.201404792.
- Warren C.J., Sawyer S.L. How host genetics dictates successful viral zoonosis. PLoS Biol. 2019; 17(4): e3000217. https://doi.org/10.1371/journal.pbio.3000217.
- Edenborough K.M., Bokelmann M., Lander A., Couacy-Hymann E., Lechner J., Drechsel O., et al. Dendritic cells generated from Mops condylurus, a likely filovirus reservoir host, are susceptible to and activated by Zaire ebolavirus infection. Front. Immunol. 2019; 10: 2414. https://doi.org/10.3389/fimmu.2019.02414.
- Guedj J., Piorkowski G., Jacquot F., Madelain V., Nguyen T.H.T., Rodallec A., et al. Antiviral efficacy of favipiravir against Ebola virus: A translational study in cynomolgus macaques. PLoS Med 2018; 15(3): e1002535. https://doi.org/10.1371/journal.pmed.1002535.
- Heymann D.L., Weisfeld J.S., Webb P.A., Johnson K.M., Cairns T., Berquist H. Ebola hemorrhagic fever: Tandala, Zaire, 1977-1978 external icon. J. Infect. Dis. 1980; 142(3): 372-6. https://doi.org/10.1093/infdis/142.3.372.
- Meunier D.M., Johnson E.D., Gonzalez J.P., Georges-Courbot M.C., Madelon M.C., Georges A.J. Current serologic data on viral hemorrhagic fevers in the Central African Republic. Bull. Soc. Pathol. Exot. Filiales. 1987; 80(1): 51-61 (in French).
- Nkoghe D., Padilla C., Becquart P., Wauquier N., Moussavou G., Akue J.P., et al. Risk factors for Zaire ebolavirus-specific IgG in rural gabonese populations. J. Infect. Dis. 2011; 204 (Suppl. 3): S768-75. https://doi.org/10.1093/infdis/jir344.
- Busico K.M., Marshall K.L., Ksiazek T.G., Roels T.H., Fleerackers Y., Feldmann H., et al. Prevalence of IgG antibodies to Ebola virus in individuals during an Ebola outbreak, Democratic Republic of the Congo, 1995. J. Infect. Dis. 1999; 179(Suppl. 1): S102-7. https://doi.org/10.1086/514309.
- Becquart P., Wauquier N., Mahlakoiv T., Nkoghe D., Padilla C., Souris M., et al. High prevalence of both humoral and cellular immunity to Zaire ebolavirus among rural populations in Gabon. PLoS One. 2010; 5(2): e9126. https://doi.org/10.1371/journal.pone.0009126.
- Van der Groen G., Pattyn S.R. Measurement of antibodies to Ebola virus in human sera from N.W.-Zaire. Ann. Soc. Belg. Med. Trop. 1979; 59(1): 87-92.
- Allela L., Bourry O., Pouillot R., Delicat A., Yaba P., Kumulungui B., et al. Ebola virus antibody prevalence in dogs and human risk. Emerg. Infect. Dis. 2005; 11(3): 385-90. https://doi.org/10.3201/eid1103.040981.
- Heffernan R.T., Pambo B., Hatchett R.J., Leman P.A., Swane-poel R., Ryder R.W. Low seroprevalence of IgG antibodies to Ebola virus in an epidemic zone: Ogooue-Ivindo region, Northeastern Gabon, 1997. J. Infect. Dis. 2005; 191(6): 964-8. https://doi.org/10.1086/427994.
- Lahm S.A., Kombila M., Swanepoel R., Barnes R.F.W. Morbidity and mortality of wild animals in relation to outbreaks of Ebola haemorrhagic fever in Gabon, 1994-2003. Trans. R. Soc. Trop. Med. Hyg. 2007; 101(1): 64-78. https://doi.org/10.1016/j.trst-mh.2006.07.002.
- Georges A.J., Leroy E.M., Renaut A.A., Benissan C.T., Nabias R.J., Ngoc M.T., et al. Ebola hemorrhagic fever outbreaks in Gabon, 1994-1997: epidemiologic and health control issues. J. Infect. Dis. 1999; 179(Suppl. 1): S65-75. https://doi.org/10.1086/514290.
- Baron R.C., McCormick J.B., Zubeir O.A. Ebola virus disease in southern Sudan: hospital dissemination and intrafamilial spread. Bull. World Health Organ. 1983; 61(6): 997-1003.
- Mathiot C.C., Georges A.J., Fontenille D., Coulanges P. Antibodies to haemorrhagic fever viruses in Madagascar populations. Trans. R. Soc. Trop. Med. Hyg. 1989; 83(3): 407-9. https://doi.org/10.1016/0035-9203(89)90519-1.
- Van der Waals F.W., Pomeroy K.L., Goudsmit J., Asher D.M., Gajdusek D.C. Hemorrhagic fever virus infections in an isolated rainforest area of Central Liberia. Limitations of the indirect immunofluorescence slide test for antibody screening in Africa. Trop. Geogr Med. 1986; 38(3): 209-14.
- Bouree P., Bergmann J.F. Ebola virus infection in man: a serological and epidemiological survey in the Cameroons. Am. J. Trop. Med. Hyg. 1983; 32(6): 1465-6. https://doi.org/10.4269/ajtmh.1983.32.1465.
- Paix M.A., Poveda J.D., Malvy D., Bailly C., Merlin M., Fleury H.J. Serological study of the virus responsible for hemorrhagic fever in an urban population of Cameroon. Bull. Soc. Pathol. Exot. Filiales. 1988; 81(4): 679-82 (in French).
- Tomori O., Fabiyi A., Sorungbe A., Smith A., McCormick J.B. Viral hemorrhagic fever antibodies in Nigerian populations. Am J. Trop. Med. Hyg. 1988; 38(2): 407-10. https://doi.org/10.4269/ajtmh.1988.38.407.
- Becker S., Feldmann H., Will C., Slenczka W. Evidence for occurrence of filovirus antibodies in humans and imported monkeys: do subclinical filovirus infections occur worldwide? Med. Microbiol. Immunol. 1992; 181(1): 43-55. https://doi.org/10.1007/BF00193395.
- Johnson B.K., Ocheng D., Gichogo A., Okiro M., Libondo D., Tukei P.M., et al. Antibodies against haemorrhagic fever viruses in Kenya populations. Trans. R. Soc. Trop. Med. Hyg. 1983; 77(5): 731-3. https://doi.org/10.1016/0035-9203(83)90216-x.
- Nyakarahuka L., Schafer I.J., Balinandi S., Mulei S., Tumusiime A., Kyondo J., et al. A retrospective cohort investigation of seropreva-lence of Marburg virus and ebolaviruses in two different ecological zones in Uganda. BMC Infect. Dis. 2020; 20(1): 461. https://doi.org/10.1186/s12879-020-05187-0.
- Эйген М., Шустер П. Гиперцикл. Принципы самоорганизации макромолекул. Пер. с англ. М.: Мир; 1982.
- Zeng X., Blancett C.D., Koistinen K.A., Schellhase C.W., Bearss J.J., Radoshitzky S.R., et al. Identification and pathological characterization of persistent asymptomatic Ebola virus infection in rhesus monkeys. Nat. Microbiol. 2017; 2: 17113. https://doi.org/10.1038/nmicrobiol.2017.113.
- Deen G.F., Broutet N., Xu W., Knust B., Sesay F.R., McDonald S.L.R., et al. Ebola RNA persistence in semen of Ebola virus disease survivors - final report. N. Engl. J. Med. 2017; 377(15): 142837. https://doi.org/10.1056/NEJMoa1511410.
- Fischer W.A., Brown J., Wohl D.A., Loftis A.J., Tozay S., Reeves E., et al. Ebola virus ribonucleic acid detection in Semen more than two years after resolution of acute Ebola virus infection. Open Forum Infect. Dis. 2017; 4(3): ofx155. https://doi.org/10.1093/ofid/ofx155.
- Forrester J.V. Ebola virus and persistent chronic infection: when does replication cease? Ann. Transl. Med. 2018; 6(Suppl. 1): S39. https://doi.org/10.21037/atm.2018.09.60.
- Varkey J.B., Shantha J.G., Crozier I., Kraft C.S., Lyon G.M., MehtaA.K., et al. Persistence of Ebola virus in ocular fluid during convalescence. N. Engl. J. Med. 2015; 372(25): 2423-7. https://doi.org/10.1038/nri2940.
- MacIntyre C.R., Chughtai A.A. Recurrence and reinfection - a new paradigm for the management of Ebola virus disease. Int. J. Infect. Dis. 2016; 43: 58-61. https://doi.org/10.1016/j.ijid.2015.12.011.
Дополнительные файлы