Analysis of genetic polymorphisms and drug resistance mutations in the NS5 region of HCV genome (Flasuviricetes: Amarillovirales: Flaviviridae: Hepacivirus C) in samples obtained in 2022–2023 from HIV-infected treatment-naive residents of Altai Krai
- Authors: Lapovok I.A.1, Syrkina A.V.1, Kirichenko A.A.1, Shlykova A.V.1, Lukyanenko N.V.2, Safyanova T.V.2, Safronova A.E.2, Shevchenko V.V.2,3, Kireev D.E.1
-
Affiliations:
- Central Research Institute of Epidemiology
- Altai State Medical University (ASMU)
- Altai Regional Center for Prevention and Control of AIDS and Infectious Diseases
- Issue: Vol 70, No 3 (2025)
- Pages: 224-233
- Section: ORIGINAL RESEARCHES
- URL: https://journal-vniispk.ru/0507-4088/article/view/310660
- DOI: https://doi.org/10.36233/0507-4088-298
- EDN: https://elibrary.ru/NZBCOE
- ID: 310660
Cite item
Abstract
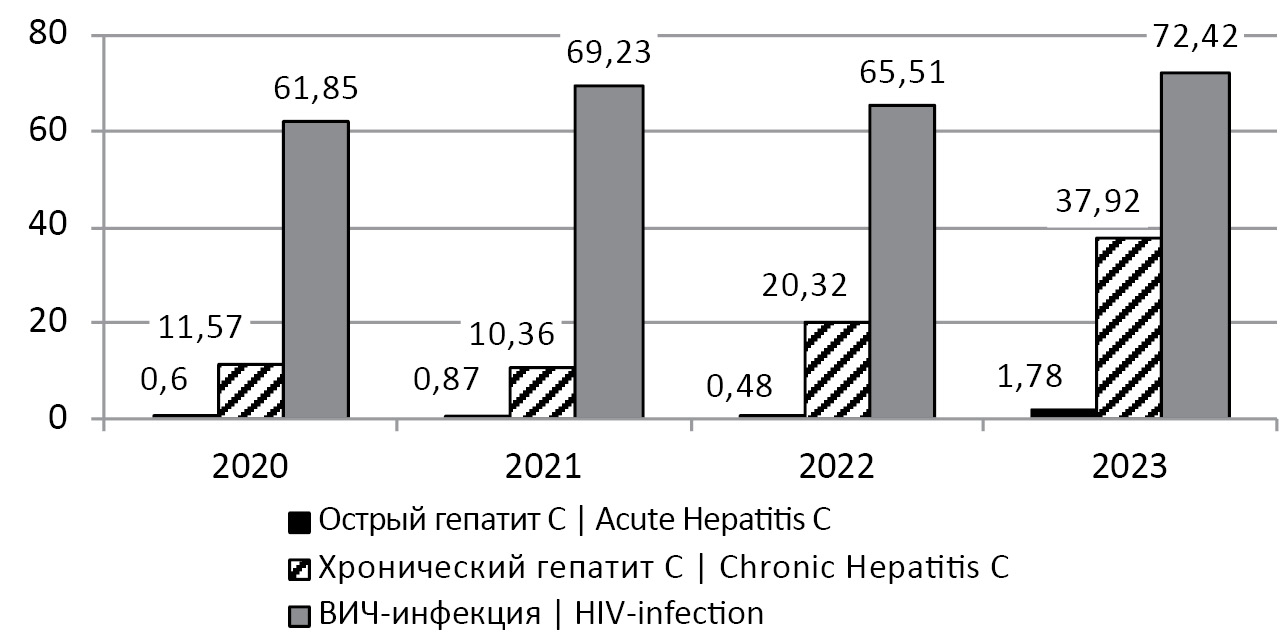
Introduction. Altai Krai is a region with an unfavorable situation of HIV-1 and HCV infection, as well as HIV-1 and HCV coinfection. Due to this, it is necessary to study the HCV genetic variants and their drug resistance (DR) to direct-acting antivirals (DAAs) in patients with HIV-1 and HCV coinfection.
Aim of the study. The analysis of HCV genome fragments encoding NS5A and NS5B proteins in samples obtained from treatment-naïve residents of Altai Krai with newly diagnosed HIV and HCV co-infection to determine the genetic variant of HCV and genetic features of the virus associated with its sensitivity to NS5A and NS5B inhibitors.
Materials and methods. Blood plasma samples (n = 286) collected in 2022–2023 from HIV-infected individuals were analyzed for HCV markers. The HCV RNA concentration was measured, nucleotide sequences of NS5A and NS5B and Core (for HCV 2k/1b samples) fragments were obtained, the subtype was determined, and DR and polymorphic positions were analyzed.
Results. Antibodies to HCV were detected in 94/286 (32.86%) samples, sequences were obtained from 52 samples. Subtypes 3a, 1b, recombinant form 2k/1b and subtype 1a were found in 28 (53.85%), 17 (32.69%), 5 (9.62%) and one (1.92%) samples, respectively. One sample harbored HCV 1b + 3a mix-infection. Reduced sensitivity (5.66%) and complete resistance (9.43%) to the NS5A inhibitor daclatasvir were most often detected. Certain gene polymorphisms were identified in the sequences.
Conclusion. Our results may indirectly indicate the increasing proportion of the HCV subtype 3a in the hepatitis C epidemic in the Altai Territory. Our data on DR and polymorphisms should be taken into account in antiviral therapy of patients.
Keywords
Full Text
##article.viewOnOriginalSite##About the authors
Ilya A. Lapovok
Central Research Institute of Epidemiology
Author for correspondence.
Email: i_lapovok@mail.ru
ORCID iD: 0000-0002-6328-1415
Cand. Sci. (Biol.), Senior Researcher, HIV diagnostic and molecular epidemiology laboratory
Russian Federation, 111123, MoscowArina V. Syrkina
Central Research Institute of Epidemiology
Email: syrkina@cmd.su
ORCID iD: 0009-0003-2733-6663
Junior Researcher, HIV diagnostic and molecular epidemiology laboratory
Russian Federation, 111123, MoscowAlina A. Kirichenko
Central Research Institute of Epidemiology
Email: kirichenko@cmd.su
ORCID iD: 0000-0002-7116-0138
Cand. Sci. (Med.), Senior Researcher, HIV diagnostic and molecular epidemiology laboratory
Russian Federation, 111123, MoscowAnastasia V. Shlykova
Central Research Institute of Epidemiology
Email: murzakova_a.v@mail.ru
ORCID iD: 0000-0002-1390-8021
Researcher, HIV diagnostic and molecular epidemiology laboratory
Russian Federation, 111123, MoscowNatalya V. Lukyanenko
Altai State Medical University (ASMU)
Email: natvalluk@mail.ru
ORCID iD: 0000-0002-0003-5145
Dr. Sci. (Med.), Professor, Department of Epidemiology, Microbiology and Virology
Russian Federation, 656038, BarnaulTatyana V. Safyanova
Altai State Medical University (ASMU)
Email: tvsafyanova@yandex.ru
ORCID iD: 0000-0003-3293-4265
Dr. Sci. (Med.), Professor, Head of the Department of Epidemiology, Microbiology and Virology
Russian Federation, 656038, BarnaulArina E. Safronova
Altai State Medical University (ASMU)
Email: safariev00@mail.ru
ORCID iD: 0009-0009-7350-6073
Resident of the Department of Epidemiology, Microbiology and Virology
Russian Federation, 656038, BarnaulValery V. Shevchenko
Altai State Medical University (ASMU); Altai Regional Center for Prevention and Control of AIDS and Infectious Diseases
Email: infecgepatit@yandex.ru
ORCID iD: 0000-0001-6282-5495
Cand. Sci. (Med.), Chief Non-staff Infectiologist, Associate Professor, Department of Epidemiology, Microbiology and Virology
Russian Federation, 656038, Barnaul; 656010, BarnaulDmitry E. Kireev
Central Research Institute of Epidemiology
Email: dmitkireev@yandex.ru
ORCID iD: 0000-0002-7896-2379
Cand. Sci. (Biol.), Head, HIV diagnostic and molecular epidemiology laboratory
Russian Federation, 111123, MoscowReferences
- Simão M., Gonçalves C. Hepatitis C virus infection in Europe. Pathogens. 2024; 13(10): 841. https://doi.org/10.3390/pathogens13100841
- Martinez M.A., Franco S. Therapy implications of hepatitis C virus genetic diversity. Viruses. 2021; 13(1): 41. https://doi.org/10.3390/v13010041
- Ostankova Yu.V., Valutite D.E., Zueva E.B., Serikova E.N., Shchemelev A.N., Boumbaly S., et al. Primary HCV drug resistance mutations in patients with newly diagnosed HIV infection. Problemy osobo opasnykh infektsii. 2020; (3): 97–105. https://elibrary.ru/laroef (in Russian)
- Valutite D., Ostankova Y., Semenov A., Lyalina L., Totolian A. Distribution of primary resistance mutations in Saint Petersburg in patients with chronic hepatitis C. Diagnostics. 2022; 12(5): 1054. https://doi.org/10.3390/diagnostics12051054
- Sulkowski M.S. Viral hepatitis and HIV coinfection. J. Hepatol. 2008; 48(2): 353–67. https://doi.org/10.1016/j.jhep.2007.11.009
- Thein H.H., Yi Q., Dore G.J., Krahn M.D. Natural history of hepatitis C virus infection in HIV-infected individuals and the impact of HIV in the era of highly active antiretroviral therapy: a meta-analysis. AIDS. 2008; 22(15): 1979–91. https://doi.org/10.1097/QAD.0b013e32830e6d51
- Wyatt C.M., Malvestutto C., Coca S.G., Klotman P.E., Parikh C.R. The impact of hepatitis C virus coinfection on HIV-related kidney disease: a systematic review and meta-analysis. AIDS. 2008; 22(14): 1799–807. https://doi.org/10.1097/QAD.0b013e32830e0152
- Vo-Quang E., Pawlotsky J.M. «Unusual» HCV genotype subtypes: origin, distribution, sensitivity to direct-acting antiviral drugs and behaviour on antiviral treatment and retreatment. Gut. 2024; 73(9): 1570–82. https://doi.org/10.1136/gutjnl-2024-332177
- Kichatova V.S., Karlsen A.A., Isaeva O.V., Solonin S.A., Malinnikova E.Yu., Kyuregyan K.K., et al. Drug resistant variants of hepatitis C Virus genotype1B in Russia: analysis of aminoacid substitutions in NS5A and core proteins. Zhurnal infektologii. 2018; 10(4): 30–6. https://elibrary.ru/vvmeki (in Russian)
- Pimenov N., Kostyushev D., Komarova S., Fomicheva A., Urtikov A., Belaia O., et al. Epidemiology and genotype distribution of hepatitis C virus in Russia. Pathogens. 2022; 11(12): 1482. https://doi.org/10.3390/pathogens11121482
- Akimov I.A., Timofeev D.I., Mavzyutov A.R., Ivanov M.K. Detection of circulating HCV recombinant form rf1_2k/1b in blood serum of patients by real-time RT-PCR. Klinicheskaya laboratornaya diagnostika. 2021; 66(2): 122–8. https://elibrary.ru/vvobzb (in Russian)
- Kalinina O., Norder H., Mukomolov S., Magnius L.O. A natural intergenotypic recombinant of hepatitis C virus identified in St. Petersburg. J. Virol. 2002; 76(8): 4034–43. https://doi.org/10.1128/jvi.76.8.4034-4043.2002
- Mushtaq S., Hashmi A.H., Khan A., Asad Raza Kazmi S.M., Manzoor S. Emergence and Persistence of Resistance-Associated Substitutions in HCV GT3 Patients Failing Direct-Acting Antivirals. Front. Pharmacol. 2022; 13: 894460. https://doi.org/10.3389/fphar.2022.894460
- Wang C., Valera L., Jia L., Kirk M.J., Gao M., Fridell R.A. In vitro activity of daclatasvir on hepatitis C virus genotype 3 NS5A. Antimicrob. Agents. Chemother. 2013; 57(1): 611–3. https://doi.org/10.1128/AAC.01874-12
- Fernandes Campos G.R., Ward J., Chen S., Bittar C., Rodrigues J.P.V., de Lourdes Candolo Martinelli A., et al. A novel substitution in NS5A enhances the resistance of hepatitis C virus genotype 3 to daclatasvir. J. Gen. Virol. 2021; 102(1): jgv001496. https://doi.org/10.1099/jgv.0.001496
- Mejer N., Fahnøe U., Galli A., Ramirez S., Weiland O., Benfield T., et al. Mutations identified in the hepatitis C virus (HCV) polymerase of patients with chronic HCV treated with ribavirin cause resistance and affect viral replication fidelity. Antimicrob. Agents Chemother. 2020; 64(12): e01417–20. https://doi.org/10.1128/AAC.01417-20
- Lee W.Y.J., Jones M., Wing P.A.C., Rajagopal S., Foster G.R. The A150V polymorphism of genotype 3 hepatitis C virus polymerase inhibits interferon alfa by suppressing protein kinase R activation. Cell. Mol. Gastroenterol. Hepatol. 2021; 11(4): 1163–75. https://doi.org/10.1016/j.jcmgh.2020.11.012
- Los Alamos HCV database. Available at: https://hcv.lanl.gov
- Kalaghatgi P., Sikorski A.M., Knops E., Rupp D., Sierra S., Heger E., et al. Geno2pheno [HCV] – a web-based interpretation system to support hepatitis C treatment decisions in the era of direct-acting antiviral agents. PLoS One. 2016; 11(5): e0155869. https://doi.org/10.1371/journal.pone.0155869
- Kichatova V.S., Kyuregyan K.K., Soboleva N.V., Karlsen A.A., Isaeva O.V., Isaguliants M.G., et al. Frequency of interferon-resistance conferring substitutions in amino acid positions 70 and 91 of core protein of the Russian HCV 1b isolates analyzed in the T-cell epitopic context. J. Immunol. Res. 2018; 2018: 7685371. https://doi.org/10.1155/2018/7685371
- Tamura K., Stecher G., Peterson D., Filipski A., Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol. Biol. Evol. 2013; 30(12): 2725–9. https://doi.org/10.1093/molbev/mst197
- Kati W., Koev G., Irvin M., Beyer J., Liu Y., Krishnan P., et al. In vitro activity and resistance profile of dasabuvir, a nonnucleoside hepatitis C virus polymerase inhibitor. Antimicrob. Agents Chemother. 2015; 59(3): 1505–11. https://doi.org/10.1128/AAC.04619-14
- Valutite D.E., Semenov A.V., Ostankova Yu.V., Kozlov K.V., Borisov A.G., Nazarov V.D. et al. Detection of drug resistance mutations of hepatitis C virus in patients with failure of the treatment with direct acting antivirals. Zhurnal mikrobiologii, epidemiologii i immunobiologii. 2021; 98(1): 18–27. https://elibrary.ru/aksnkx (in Russian)
Supplementary files