胃肠道间质瘤的放射组学诊断潜力:科学综述
- 作者: Martirosyan E.A.1,2, Karmazanovsky G.G.1,3, Kondratyev E.V.1, Sokolova E.A.1, Nechaev V.A.2, Kuzmina E.S.2, Galkin V.N.2, Glotov A.V.1
-
隶属关系:
- A.V. Vishnevsky National Medical Research Center of Surgery
- S.S. Yudin City Clinical Hospital
- The Russian National Research Medical University named N.I. Pirogov
- 期: 卷 6, 编号 1 (2025)
- 页面: 143-155
- 栏目: 科学评论
- URL: https://journal-vniispk.ru/DD/article/view/310058
- DOI: https://doi.org/10.17816/DD631596
- ID: 310058
如何引用文章
详细
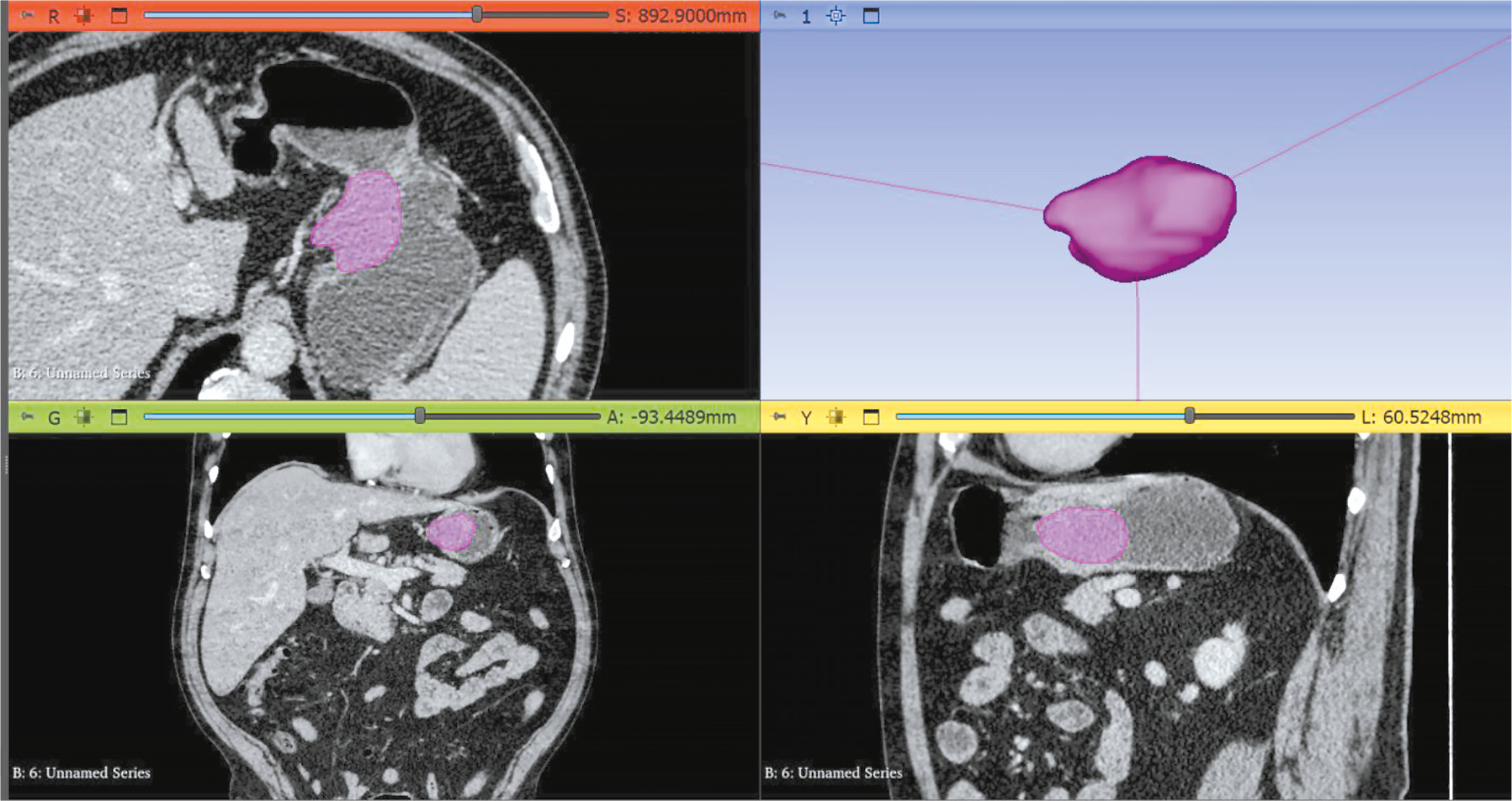
胃肠道间质瘤是最常见的胃肠道间叶性肿瘤,来源于卡哈尔氏间质细胞,约占所有胃部原发性肿瘤的80%。传统的胃肠道间质瘤诊断方法,如计算机断层扫描、内镜检查、内镜超声检查和细针穿刺活检,尽管被广泛应用,但仍存在一些缺点,包括诊断不确定性和活检的局限性。
放射组学,作为图像纹理特征分析的创新方法,被认为有潜力提高胃肠道间质瘤的诊断精度。这种方法通过对图像的数学处理来解读组织中的变化,这是人眼无法直接看到的,从而有助于更早期地发现肿瘤。
本文评估了当前胃肠道间质瘤诊断方法的优缺点,并探讨了放射组学在提高诊断效果方面的潜力。综述旨在确定最佳的应用方式和未来研究的前景方向。
作者简介
Elina A. Martirosyan
A.V. Vishnevsky National Medical Research Center of Surgery; S.S. Yudin City Clinical Hospital
编辑信件的主要联系方式.
Email: robatik2009@mail.ru
ORCID iD: 0000-0002-1854-9638
SPIN 代码: 8006-8917
俄罗斯联邦, Moscow; Moscow
Grigory G. Karmazanovsky
A.V. Vishnevsky National Medical Research Center of Surgery; The Russian National Research Medical University named N.I. Pirogov
Email: karmazanovsky@ixv.ru
ORCID iD: 0000-0002-9357-0998
SPIN 代码: 5964-2369
MD, Dr. Sci. (Medicine), Professor, academician of the Russian Academy of Sciences
俄罗斯联邦, Moscow; MoscowEvgeny V. Kondratyev
A.V. Vishnevsky National Medical Research Center of Surgery
Email: kondratev@ixv.ru
ORCID iD: 0000-0001-7070-3391
SPIN 代码: 2702-6526
MD, Cand. Sci. (Medicine)
俄罗斯联邦, MoscowElena A. Sokolova
A.V. Vishnevsky National Medical Research Center of Surgery
Email: elena83.sokolova@yandex.ru
ORCID iD: 0000-0002-5667-7833
SPIN 代码: 9197-6568
俄罗斯联邦, Moscow
Valentin A. Nechaev
S.S. Yudin City Clinical Hospital
Email: nechaevva1@zdrav.mos.ru
ORCID iD: 0000-0002-6716-5593
SPIN 代码: 2527-0130
MD, Cand. Sci. (Medicine)
俄罗斯联邦, MoscowEvgeniya S. Kuzmina
S.S. Yudin City Clinical Hospital
Email: kuz011@mail.ru
ORCID iD: 0009-0007-2856-5176
SPIN 代码: 9668-5733
俄罗斯联邦, Moscow
Vsevolod N. Galkin
S.S. Yudin City Clinical Hospital
Email: galkinvn2@zdrav.mos.ru
ORCID iD: 0000-0002-6619-6179
SPIN 代码: 3148-4843
MD, Dr. Sci. (Medicine), Professor
俄罗斯联邦, MoscowAndrey V. Glotov
A.V. Vishnevsky National Medical Research Center of Surgery
Email: andrew.glotov@mail.ru
ORCID iD: 0000-0002-6904-9318
SPIN 代码: 4947-4382
俄罗斯联邦, Moscow
参考
- Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Seminars in Diagnostic Pathology. 2006;23(2):70–83. doi: 10.1053/j.semdp.2006.09.001
- Søreide K, Sandvik OM, Søreide JA, et al. Global epidemiology of gastrointestinal stromal tumours (GIST): a systematic review of population-based cohort studies. Cancer Epidemiology. 2016;40:39–46. doi: 10.1016/j.canep.2015.10.031
- Corless CL, Barnett CM, Heinrich MC. Gastrointestinal stromal tumours: origin and molecular oncology. Nature Reviews Cancer. 2011;11(12):865–878. doi: 10.1038/nrc3143
- Menge F, Jakob J, Kasper B, et al. Clinical presentation of gastrointestinal stromal tumors. Visceral Medicine. 2018;34(5):335–340. doi: 10.1159/000494303
- Korzheva IYu, Chernekhovskaya NE, Volova AV, et al. Gastrointestinal stromal tumors — treatment and diagnostic algorithm. Experimental and Clinical Gastroenterology. 2023;(5):108–113. doi: 10.31146/1682-8658-ecg-213-5-108-113 EDN: KEHFAO
- Fletcher CDM, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Human Pathology. 2002;33(5):459–465. doi: 10.1053/hupa.2002.123545
- Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Human Pathology. 2008;39(10):1411–1419. doi: 10.1016/j.humpath.2008.06.025
- Hong X, Choi H, Loyer EM, et al. Gastrointestinal stromal tumor: role of CT in diagnosis and in response evaluation and surveillance after treatment with Imatinib. RadioGraphics. 2006;26(2):481–495. doi: 10.1148/rg.262055097
- Inoue A, Ota S, Yamasaki M, et al. Gastrointestinal stromal tumors: a comprehensive radiological review. Japanese Journal of Radiology. 2022;40(11):1105–1120. doi: 10.1007/s11604-022-01305-x EDN: DJOHPD
- Dimitrakopoulou-Strauss A, Ronellenfitsch U, Cheng C, et al. Imaging therapy response of gastrointestinal stromal tumors (GIST) with FDG PET, CT and MRI: a systematic review. Clinical and Translational Imaging. 2017;5(3):183–197. doi: 10.1007/s40336-017-0229-8 EDN: YEZTPW
- Bano S, Puri SK, Upreti L, et al. Gastrointestinal stromal tumors (GISTS): an imaging perspective. Japanese Journal of Radiology. 2011;30(2):105–115. doi: 10.1007/s11604-011-0020-0 EDN: XAZRKK
- Horton KM, Juluru K, Montogomery E, Fishman EK. Computed tomography imaging of gastrointestinal stromal tumors with pathology correlation. Journal of Computer Assisted Tomography. 2004;28(6):811–817. doi: 10.1097/00004728-200411000-00014
- Martirosyan EA, Karmazanovsky GG, Sokolova EA, et al. Submucosal gastric lesions: a CECT-based tool for differential diagnosis between gastrointestinal stromal tumor and leiomyoma. Medical Visualization. 2020;24(4):27–41. doi: 10.24835/1607-0763-2020-4-27-41 EDN: NDYYRO
- Choi YR, Kim SH, Kim S-A, et al. Differentiation of large (≥5 cm) gastrointestinal stromal tumors from benign subepithelial tumors in the stomach: radiologists’ performance using CT. European Journal of Radiology. 2014;83(2):250–260. doi: 10.1016/j.ejrad.2013.10.028
- Xu JX, Ding QL, Lu YF, et al. A scoring model for radiologic diagnosis of gastric leiomyomas (GLMs) with contrast-enhanced computed tomography (CE-CT): differential diagnosis from gastrointestinal stromal tumors (GISTs). European Journal of Radiology. 2021;134:109395. doi: 10.1016/j.ejrad.2020.109395 EDN: UNDSRT
- Yan M, Liu Y, You H, et al. Differentiation of small gastrointestinal stromal tumor and gastric leiomyoma with contrast-enhanced CT. Journal of Healthcare Engineering. 2023;2023:1–6. doi: 10.1155/2023/6423617 EDN: YWPQDU
- Chen Z, Yang J, Sun J, Wang P. Gastric gastrointestinal stromal tumours (2–5 cm): correlation of CT features with malignancy and differential diagnosis. European Journal of Radiology. 2020;123:108783. doi: 10.1016/j.ejrad.2019.108783 EDN: PEEWLT
- Iannicelli E, Carbonetti F, Federici GF, et al. Evaluation of the relationships between computed tomography features, pathological findings, and prognostic risk assessment in gastrointestinal stromal tumors. Journal of Computer Assisted Tomography. 2017;41(2):271–278. doi: 10.1097/rct.0000000000000499
- Joensuu H, Fletcher C, Dimitrijevic S, et al. Management of malignant gastrointestinal stromal tumours. The Lancet Oncology. 2002;3(11):655–664. doi: 10.1016/s1470-2045(02)00899-9
- Hunt GC, Smith PP, Faigel DO. Yield of tissue sampling for submucosal lesions evaluated by EUS. Gastrointestinal Endoscopy. 2003;57(1):68–72. doi: 10.1067/mge.2003.34
- Park JE, Kim D, Kim HS, et al. Quality of science and reporting of radiomics in oncologic studies: Room for improvement according to radiomics quality score and TRIPOD statement. European Radiology. 2020;30(1):523–536. doi: 10.1007/s00330-019-06360-z EDN: RYQMNX
- Aerts HJWL, Velazquez ER, Leijenaar RT, et al. Corrigendum: Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nature Communications. 2014;5:4644. doi: 10.1038/ncomms5644
- Scapicchio C, Gabelloni M, Barucci A, et al. A deep look into radiomics. La radiologia medica. 2021;126(10):1296–1311. doi: 10.1007/s11547-021-01389-x EDN: CFTFXK
- Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278(2):563–577. doi: 10.1148/radiol.2015151169
- Lambin P, Leijenaar RTH, Deist TM, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nature Reviews Clinical Oncology. 2017;14(12):749–762. doi: 10.1038/nrclinonc.2017.141
- Yip SS, Aerts HJ. Applications and limitations of radiomics. Physics in Medicine and Biology. 2016;61(13):R150–R166. doi: 10.1088/0031-9155/61/13/R150
- Ganeshan B, Abaleke S, Young RC, et al. Texture analysis of non-small cell lung cancer on unenhanced computed tomography: initial evidence for a relationship with tumour glucose metabolism and stage. Cancer Imaging. 2010;10(1):137–143. doi: 10.1102/1470-7330.2010.0021
- Bachet JB, Hostein I, Le Cesne A, et al. Prognosis and predictive value of KIT exon 11 deletion in GISTs. British Journal of Cancer. 2009;101(1):7–11. doi: 10.1038/sj.bjc.6605117 EDN: NXUXXL
- Wang M, Xu J, Zhao W, et al. Prognostic value of mutational characteristics in gastrointestinal stromal tumors: a single-center experience in 275 cases. Medical Oncology. 2013;31(1):819. doi: 10.1007/s12032-013-0819-x EDN: AAFFTP
- Liu X, Yin Y, Wang X, et al. Gastrointestinal stromal tumors: associations between contrast-enhanced CT images and KIT exon 11 gene mutation. Annals of Translational Medicine. 2021;9(19):1496–1496. doi: 10.21037/atm-21-3811 EDN: XKKHIX
- Xu F, Ma X, Wang Y, et al. CT texture analysis can be a potential tool to differentiate gastrointestinal stromal tumors without KIT exon 11 mutation. European Journal of Radiology. 2018;107:90–97. doi: 10.1016/j.ejrad.2018.07.025
- Guo C, Zhou H, Chen X, Feng Z. Computed tomography texture-based models for predicting KIT exon 11 mutation of gastrointestinal stromal tumors. Heliyon. 2023;9(10):e20983. doi: 10.1016/j.heliyon.2023.e20983 EDN: OMPRCQ
- Zhang QW, Zhang RY, Yan ZB, et al. Personalized radiomics signature to screen for KIT-11 mutation genotypes among patients with gastrointestinal stromal tumors: a retrospective multicenter study. Journal of Translational Medicine. 2023;21(1):726. doi: 10.1186/s12967-023-04520-w EDN: MZEKJH
- Künstlinger H, Huss S, Merkelbach-Bruse S, et al. Gastrointestinal stromal tumors with KIT exon 9 mutations. American Journal of Surgical Pathology. 2013;37(11):1648–1659. doi: 10.1097/pas.0b013e3182986b88
- Gastrointestinal Stromal Tumor Meta-Analysis Group (MetaGIST). Comparison of two doses of Imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1 640 patients. Journal of Clinical Oncology. 2010;28(7):1247–1253. doi: 10.1200/JCO.2009.24.2099
- Wei Y, Lu Z, Ren Y. Predictive value of a radiomics nomogram model based on contrast-enhanced computed tomography for KIT exon 9 gene mutation in gastrointestinal stromal tumors. Technology in Cancer Research & Treatment. 2023;22:153303382311812. doi: 10.1177/15330338231181260 EDN: XTXBRZ
- Serrano C, Álvarez R, Carrasco JA, et al. SEOM-GEIS clinical guideline for gastrointestinal stromal tumors (2022). Clinical and Translational Oncology. 2023;25(9):2707–2717. doi: 10.1007/s12094-023-03177-7 EDN: AKQBYR
- Jakob J, Salameh R, Wichmann D, et al. Needle tract seeding and abdominal recurrence following pre-treatment biopsy of gastrointestinal stromal tumors (GIST): results of a systematic review. BMC Surgery. 2022;22(1):202. doi: 10.1186/s12893-022-01648-2 EDN: ACKOXX
- Zhang L, Kang L, Li G, et al. Computed tomography-based radiomics model for discriminating the risk stratification of gastrointestinal stromal tumors. La radiologia medica. 2020;125(5):465–473. doi: 10.1007/s11547-020-01138-6 EDN: QGFJNL
- Wang C, Li H, Jiaerken Y, et al. Building CT radiomics-based models for preoperatively predicting malignant potential and mitotic count of gastrointestinal stromal tumors. Translational Oncology. 2019;12(9):1229–1236. doi: 10.1016/j.tranon.2019.06.005
- Chen T, Ning Z, Xu L, et al. Radiomics nomogram for predicting the malignant potential of gastrointestinal stromal tumours preoperatively. European Radiology. 2019;29(3):1074–1082. doi: 10.1007/s00330-018-5629-2 EDN: RGIYYW
- Chu H, Pang P, He J, et al. Value of radiomics model based on enhanced computed tomography in risk grade prediction of gastrointestinal stromal tumors. Scientific Reports. 2021;11(1):12009. doi: 10.1038/s41598-021-91508-5 EDN: UBTXKP
- Zhou C, Duan X, Zhang X, et al. Predictive features of CT for risk stratifications in patients with primary gastrointestinal stromal tumour. European Radiology. 2015;26(9):3086–3093. doi: 10.1007/s00330-015-4172-7 EDN: YZBWHO
- O’Neill AC, Shinagare AB, Kurra V, et al. Assessment of metastatic risk of gastric gist based on treatment-naïve CT features. European Journal of Surgical Oncology (EJSO). 2016;42(8):1222–1228. doi: 10.1016/j.ejso.2016.03.032
- Li H, Ren G, Cai R, et al. A correlation research of ki67 index, CT features, and risk stratification in gastrointestinal stromal tumor. Cancer Medicine. 2018;7(9):4467–4474. doi: 10.1002/cam4.1737
- Yang L, Ma CF, Li Y, et al. Application of radiomics in predicting the preoperative risk stratification of gastric stromal tumors. Diagnostic and Interventional Radiology. 2022;28(6):532–539. doi: 10.5152/dir.2022.21033 EDN: DOWKAB
- Wang Y, Wang Y, Ren J, et al. Malignancy risk of gastrointestinal stromal tumors evaluated with noninvasive radiomics: a multi-center study. Frontiers in Oncology. 2022;12:966743. doi: 10.3389/fonc.2022.966743 EDN: DICNWT
- Lin JX, Wang FH, Wang ZK, et al. Prediction of the mitotic index and preoperative risk stratification of gastrointestinal stromal tumors with CT radiomic features. La radiologia medica. 2023;128(6):644–654. doi: 10.1007/s11547-023-01637-2 EDN: PBJVAL
- Wang P, Yan J, Qiu H, et al. A radiomics-clinical combined nomogram-based on non-enhanced CT for discriminating the risk stratification in GISTS. Journal of Cancer Research and Clinical Oncology. 2023;149(14):12993–13003. doi: 10.1007/s00432-023-05170-7 EDN: SCPQMA
- Fu J, Fang M, Dong D, et al. Heterogeneity of metastatic gastrointestinal stromal tumor on texture analysis: DWI texture as potential biomarker of overall survival. European Journal of Radiology. 2020;125:108825. doi: 10.1016/j.ejrad.2020.108825 EDN: QLLUWS
- Yang L, Zheng T, Dong Y, et al. MRI texture-based models for predicting mitotic index and risk classification of gastrointestinal stromal tumors. Journal of Magnetic Resonance Imaging. 2021;53(4):1054–1065. doi: 10.1002/jmri.27390 EDN: CHGAIP
- Mao H, Zhang B, Zou M, et al. MRI-based Radiomics models for predicting risk classification of gastrointestinal stromal tumors. Frontiers in Oncology. 2021;11:631927. doi: 10.3389/fonc.2021.631927 EDN: DHDMQA
- Yang L, Du D, Zheng T, et al. Deep learning and radiomics to predict the mitotic index of gastrointestinal stromal tumors based on multiparametric MRI. Frontiers in Oncology. 2022;12:948557. doi: 10.3389/fonc.2022.948557 EDN: NGMQKM
- Zhuo M, Guo J, Tang Y, et al. Ultrasound radiomics model-based nomogram for predicting the risk stratification of gastrointestinal stromal tumors. Frontiers in Oncology. 2022;12:905036. doi: 10.3389/fonc.2022.905036 EDN: TZAWCU
- Jia X, Wan L, Chen X, et al. Risk stratification for 1- to 2-cm gastric gastrointestinal stromal tumors: visual assessment of CT and EUS high-risk features versus CT radiomics analysis. European Radiology. 2022;33(4):2768–2778. doi: 10.1007/s00330-022-09228-x EDN: TJNIGC
- Seidal T., Edvardsson H. Expression of c-KIT (CD117) and KI67 provides information about the possible cell of origin and clinical course of gastrointestinal stromal tumours. Histopathology. 1999;34(5):416–424. doi: 10.1046/j.1365-2559.1999.00643.x
- Li J, Wang AR, Chen XD, et al. Ki67 for evaluating the prognosis of gastrointestinal stromal tumors: a systematic review and meta-analysis. Oncology Letters. 2022;23(6):189. doi: 10.3892/ol.2022.13309 EDN: YOADXG
- Zhang Q, Gao Y, Zhang R, et al. Personalized CT-based radiomics nomogram preoperative predicting ki-67 expression in gastrointestinal stromal tumors: a multicenter development and validation cohort. Clinical and Translational Medicine. 2020;9(1):12. doi: 10.1186/s40169-020-0263-4 EDN: GQEWHE
- Feng Q, Tang B, Zhang Y, Liu X. Prediction of the ki-67 expression level and prognosis of gastrointestinal stromal tumors based on CT radiomics nomogram. International Journal of Computer Assisted Radiology and Surgery. 2022;17(6):1167–1175. doi: 10.1007/s11548-022-02575-6 EDN: WMCKNC
- Liu M, Bian J. Radiomics signatures based on contrast-enhanced CT for preoperative prediction of the ki-67 proliferation state in gastrointestinal stromal tumors. Japanese Journal of Radiology. 2023;41(7):741–751. doi: 10.1007/s11604-023-01391-5 EDN: MGYVDQ
- Zhang XD, Zhang L, Gong T, et al. A combined radiomic model distinguishing GISTs from leiomyomas and schwannomas in the stomach based on endoscopic ultrasonography images. J Appl Clin Med Phys. 2023;24(7):e14023. doi: 10.1002/acm2.14023 EDN: GVPUPG
- Starmans MP, Timbergen MJ, Vos M, et al. Differential diagnosis and molecular stratification of gastrointestinal stromal tumors on CT images using a radiomics approach. Journal of Digital Imaging. 2022;35(2):127–136. doi: 10.1007/s10278-022-00590-2 EDN: FZSWKG
- Wang FH, Zheng HL, Li JT, et al. Prediction of recurrence-free survival and adjuvant therapy benefit in patients with gastrointestinal stromal tumors based on radiomics features. La radiologia medica. 2022;127(10):1085–1097. doi: 10.1007/s11547-022-01549-7 EDN: MDONPE
- Ao W, Cheng G, Lin B, et al. A novel CT-based radiomic nomogram for predicting the recurrence and metastasis of gastric stromal tumors. American journal of cancer research. 2021;11(6):3123–3134.
补充文件