放射组学和剂量组学在寻找肺辐射损伤预测因数方面的应用经验
- 作者: Nudnov N.V.1,2,3, Sotnikov V.M.1, Ivannikov M.E.1, Shakhvalieva E.S.1, Borisov A.A.1, Ledenev V.V.4, Smyslov A.Y.1, Ananina A.V.1
-
隶属关系:
- Russian Scientific Center of Roentgenoradiology
- Russian Medical Academy of Continuous Professional Education
- Peoples’ Friendship University of Russia
- Central Clinical Military Hospital
- 期: 卷 5, 编号 4 (2024)
- 页面: 752-764
- 栏目: 原创性科研成果
- URL: https://journal-vniispk.ru/DD/article/view/309834
- DOI: https://doi.org/10.17816/DD629352
- ID: 309834
如何引用文章
详细
论证。放射组学是一种基于机器学习从数字医学影像中提取、分析和解释定量特征的技术。近年来,“剂量组学”一词在文献中越来越常见,标志着放射组学的新方向。剂量组学是一种对放射治疗过程中辐射剂量分布计划进行纹理分析的方法。剂量组学领域已发表的大多数研究都致力于其在预测辐射引起的肺损伤中的应用。
目的 — 利用放射组学的纹理方法和肺部图像的剂量组学分析,以及计算机断层扫描获得的胸部软组织,从而确定肺部辐射损伤的预测因数(生物标志物)。
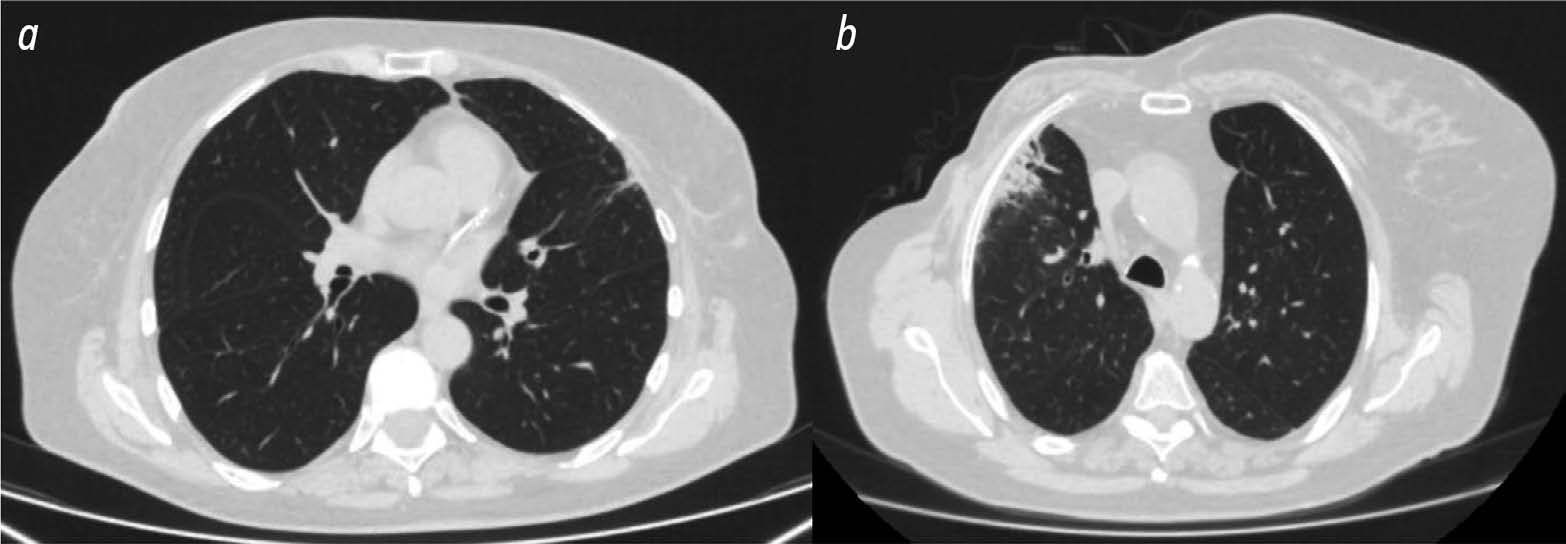
材料和方法。研究中,使用了36名接受术后适形放射治疗的乳腺癌妇女的数据。根据放疗后肺部变化的程度回顾性地将患者分为两组。使用3D Slicer软件对所有患者在放疗计划阶段获得的CT扫描结果和辐射剂量分布计划进行分析,该软件具有上传研究区域的放射组学和剂量组学指标的功能。选择照射一侧的胸部软组织和肺部区域作为研究区域,剂量负荷分别超过3 Gy和10 Gy。
结果。第一组包括13名放疗后肺部变化最小的患者,第二组包括23名放疗后肺纤维化的患者。在剂量负荷超过3 Gy的照射侧肺区,三项放射组学指标和一项剂量组学指标在患者组间存在显著统计学差异。在剂量负荷超过10 Gy的照射侧肺区,12项放射组学指标和1项剂量组学指标存在显著统计学差异。在照射一侧的胸部软组织区域,18项放射组学指标和4项剂量组学指标存在显著差异。
结论。研究结果表明,在乳腺癌放疗后、肺部放疗后微小变化和放疗后肺纤维化的患者中,一 系列的放射组学和剂量组学指标存在统计学差异。我们根据纹理分析确定的预测因数(生物标志物)可用于预测放射后肺损伤,并确定发生肺损伤的发展风险较高的患者。
作者简介
Nikolay V. Nudnov
Russian Scientific Center of Roentgenoradiology; Russian Medical Academy of Continuous Professional Education; Peoples’ Friendship University of Russia
编辑信件的主要联系方式.
Email: nudnov@rncrr.ru
ORCID iD: 0000-0001-5994-0468
SPIN 代码: 3018-2527
MD, Dr. Sci. (Medicine), Professor
俄罗斯联邦, Moscow; Moscow; MoscowVladimir M. Sotnikov
Russian Scientific Center of Roentgenoradiology
Email: vmsotnikov@mail.ru
ORCID iD: 0000-0003-0498-314X
SPIN 代码: 3845-0154
MD, Dr. Sci. (Medicine), Professor
俄罗斯联邦, MoscowMikhail E. Ivannikov
Russian Scientific Center of Roentgenoradiology
Email: ivannikovmichail@gmail.com
ORCID iD: 0009-0007-0407-0953
SPIN 代码: 3419-2977
MD
俄罗斯联邦, MoscowElina S.-A. Shakhvalieva
Russian Scientific Center of Roentgenoradiology
Email: shelina9558@gmail.com
ORCID iD: 0009-0000-7535-8523
MD
俄罗斯联邦, MoscowAleksandr A. Borisov
Russian Scientific Center of Roentgenoradiology
Email: aleksandrborisov10650@gmail.com
ORCID iD: 0000-0003-4036-5883
SPIN 代码: 4294-4736
MD
俄罗斯联邦, MoscowVasiliy V. Ledenev
Central Clinical Military Hospital
Email: Ledenevvv007@gmail.com
ORCID iD: 0000-0002-2856-2107
SPIN 代码: 2791-0329
MD, Cand. Sci. (Medicine)
俄罗斯联邦, MoscowAleksei Yu. Smyslov
Russian Scientific Center of Roentgenoradiology
Email: smyslov.ay@gmail.com
ORCID iD: 0000-0002-6409-6756
SPIN 代码: 9341-0037
Cand. Sci. (Engineering)
俄罗斯联邦, MoscowAlina V. Ananina
Russian Scientific Center of Roentgenoradiology
Email: vastruhina.a.v@yandex.ru
ORCID iD: 0009-0002-4562-9729
SPIN 代码: 9699-7690
俄罗斯联邦, Moscow
参考
- Khmelevsky EV, Kaprin AD. The state of a radiotherapy service in Russia: Comparative analysis and prospects for development. P.A. Herzen Journal of Oncology. 2017;6(4):38-41. EDN: ZFCHGJ doi: 10.17116/onkolog20176438-41
- Kuipers ME, van Doorn Wink KCJ, Hiemstra PS, Slats AM. Predicting radiation induced lung injury in lung cancer patients — challenges and opportunities: Predicting radiation induced lung injury. Int J Radiat Oncol Biol Phys. 2023;118(3):639–649. doi: 10.1016/j.ijrobp.2023.10.044
- Mayerhoefer ME, Materka A, Langs G, et al. Introduction to Radiomics. J Nucl Med. 2020;61(4):488–495. doi: 10.2967/jnumed.118.222893
- Radiomic Features: pyradiomics v3.0.1.post15+g2791e23 documentation [Internet]. [cited 25 Nov 2023]. Available from: https://pyradiomics.readthedocs.io/en/latest/features.html#.
- Avanzo M, Stancanello J, Pirrone G, Sartor G. Radiomics and deep learning in lung cancer. Strahlenther Onkol. 2020;196(10):879–887. doi: 10.1007/s00066-020-01625-9
- Gabryś HS, Buettner F, Sterzing F, et al. Design and selection of machine learning methods using radiomics and dosiomics for normal tissue complication probability modeling of xerostomia. Front Oncol. 2018;8:35. doi: 10.3389/fonc.2018.00035
- Solodkiy VA, Nudnov NV, Ivannikov ME, et al. Dosiomics in the analysis of medical images and prospects for its use in clinical practice. Digital Diagnostics. 2023;4(3):340–355. EDN: EQRWGJ doi: 10.17816/DD420053
- Arroyo Hernández M, Maldonado F, Lozano Ruiz F, et al. Radiation induced lung injury: Current evidence. BMC Pulm Med. 2021;21(1):9. doi: 10.1186/s12890-020-01376-4
- Rahi MS, Parekh J, Pednekar P, et al. Radiation Induced Lung Injury — Current Perspectives and Management. Clin Pract. 2021;11(3):410–429. doi: 10.3390/clinpract11030056
- Yan Y, Fu J, Kowalchuk RO, et al. Exploration of radiation induced lung injury, from mechanism to treatment: a narrative review. Transl Lung Cancer Res. 2022;11(2):307–322. doi: 10.21037/tlcr-22-108
- Gladilina IA, Shabanov MA, Kravets OA, et al. Radiation Induced Lung Injury. Journal of oncology: diagnostic radiology and radiotherapy. 2020;3(2):9–18. EDN: SKOAAY doi: 10.37174/2587-7593-2020-3-2-9-18
- Nudnov NV, Sotnikov VM, Ledenev VV, Baryshnikova DV. Features a Qualitative Assessment of Radiation Induced Lung Damage by CT. Medical Visualization. 2016;(1):39–46. EDN: VWOIIB
- Ledenev VV. Methodology for quantitative assessment of radiation damage to lungs in cancer patients using CT [dissertation]. Moscow, 2023. Available from: https://www.rncrr.ru/nauka/dissertatsionnyysovet/obyavleniyaozashchitakh/upload%202023/Леденев_ Диссертация.pdf (In Russ.) EDN: YBWROM
- Zhou C, Yu J. Chinese expert consensus on diagnosis and treatment of radiation pneumonitis. Prec Radiat Oncol. 2022;6(3):262–271. doi: 10.1002/pro6.1169
- Konkol M, Śniatała P, Milecki P. Radiation induced lung injury — what do we know in the era of modern radiotherapy? Rep Pract Oncol Radiother. 2022;27(3):552–565. doi: 10.5603/RPOR.a2022.0046
- Shaymuratov RI. Radiation induced lung injury. A review. The Bulletin of Contemporary Clinical Medicine. 2020;13(3):63–73. EDN: BIZZHU doi: 10.20969/VSKM.2020.13(3).63-73
- D Slicer image computing platform [Internet]. [cited 25 Nov 2023]. Available from: https://www.slicer.org/
- Wang L, Gao Z, Li C, et al. Computed Tomography Based Delta Radiomics Analysis for Discriminating Radiation Pneumonitis in Patients With Esophageal Cancer After Radiation Therapy. Int J Radiat Oncol Biol Phys. 2021;111(2):443–455. doi: 10.1016/j.ijrobp.2021.04.047
- Begosh Mayne D, Kumar SS, Toffel S, et al. The dose response characteristics of four NTCP models: using a novel CT-based radiomic method to quantify radiation-induced lung density changes. Sci Rep. 2020;10(1):10559. doi: 10.1038/s41598-020-67499-0
- Korpela E, Liu SK. Endothelial perturbations and therapeutic strategies in normal tissue radiation damage. Radiat Oncol. 2014;9:266. doi: 10.1186/s13014-014-0266-7
- Zhao L, Sheldon K, Chen M, et al. The predictive role of plasma TGF-beta1 during radiation therapy for radiation induced lung toxicity deserves further study in patients with non small cell lung cancer. Lung Cancer. 2008;59(2):232–239. doi: 10.1016/j.lungcan.2007.08.010
- Chen S, Zhou S, Zhang J, et al. A neural network model to predict lung radiation induced pneumonitis. Med Phys. 2007;34(9):3420–3427. doi: 10.1118/1.2759601
- Jain V, Berman AT. Radiation Pneumonitis: Old Problem, New Tricks. Cancers (Basel). 2018;10(7):222. doi: 10.3390/cancers10070222
- Huang Y, Feng A, Lin Y, et al. Radiation pneumonitis prediction after stereotactic body radiation therapy based on 3D dose distribution: Dosiomics and/or deep learning-based radiomics features. Radiat Oncol. 2022;17(1):188. doi: 10.1186/s13014-022-02154-8
- Zhang Z, Wang Z, Yan M, et al. Radiomics and dosiomics signature from whole lung predicts radiation pneumonitis: A model development study with prospective external validation and decision curve analysis. Int J Radiat Oncol Biol Phys. 2023;115(3):746–758. doi: 10.1016/j.ijrobp.2022.08.047
- Puttanawarut C, Sirirutbunkajorn N, Khachonkham S, et al. Biological dosiomic features for the prediction of radiation pneumonitis in esophageal cancer patients. Radiat Oncol. 2021;16(1):220. doi: 10.1186/s13014-021-01950-y
- Liang B, Yan H, Tian Y, et al. Dosiomics: Extracting 3D spatial features from dose distribution to predict incidence of radiation pneumonitis. Front Oncol. 2019;(9):269.doi: 10.3389/fonc.2019.00269
- Liang B, Tian Y, Chen X, et al. Prediction of radiation pneumonitis with dose distribution: A convolutional neural network (CNN) based model. Front Oncol. 2020;9:1500. doi: 10.3389/fonc.2019.01500
- Adachi T, Nakamura M, Shintani T, et al. Multi institutional dose segmented dosiomic analysis for predicting radiation pneumonitis after lung stereotactic body radiation therapy. Med Phys. 2021;48(4):1781–1791. doi: 10.1002/mp.14769
- Zheng X, Guo W, Wang Y, et al. Multi omics to predict acute radiation esophagitis in patients with lung cancer treated with intensity modulated radiation therapy. Eur J Med Res. 2023;28(1):126. doi: 10.1186/s40001-023-01041-6
补充文件